Injuries to the lower limb are often sustained in motor vehicle and sporting accidents
In cases where the bone is broken but there is no break in the skin (a closed fracture), surgery can be carried out by an orthopaedic surgeon alone. However, in open fracture cases, where the bone has broken through the overlying tissue, orthopaedic surgeons need to work alongside plastic surgeons to repair the injury.
Open fractures are at much greater risk of infections, delayed healing of the bone, and delayed return to function. Established bone infection can be difficult to treat. At worst amputaion of the limb might be required. Open fractures need to be managed using techniques that allow early wound closure, thus converting them to closed fractures. This approach minimises the risks normally associated with open fractures.
Wherever possible, patients with open fractures of the lower limb should be treated in specialist centres where a combination of specialist orthopaedic and plastic surgery is available. In these centres, surgical teams can produce combined plans for the management of both bone and soft tissue, and can work towards creating the best possible healing environment for the healing of the fracture and overall care of the patient.
What surgery is available, and what techniques are involved?
Definitive standards released in 2009 state that patients with these injuries should be transferred to the appropriate specialist centre. You can view the standards here
At the first operation the plastic surgeon clears the wound of dead or damaged soft tissue, while the orthopaedic surgeon clears away any damaged, non-viable bone. This procedure, also known as wound excision, is critical, as any dead tissue or bone remnants that are left in the wound can lead to infection. Once the wound is clean, the plastic and orthopaedic surgeon will then decide together on the best treatment plan for the patient.
Once the wound has been excised, further treatment involves two key stages:
 1. First, the orthopaedic surgeon repairs the broken bone. This can be a simple fixation procedure, or it can be highly complex depending on the nature of the injury.
1. First, the orthopaedic surgeon repairs the broken bone. This can be a simple fixation procedure, or it can be highly complex depending on the nature of the injury.
Cases where the bone has been shattered, for example, are much more difficult to repair than a straightforward break. The surgeon may need to trim the bone or make a surgical break in order to grow the bone back together, using a circular frame.
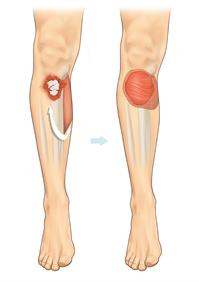
2. Secondly, once the bone has been fixed, the plastic surgeon will work to repair the damaged tissue using flap reconstruction. Flap reconstruction involves the transfer of a living piece of tissue from one part of the body to another, along with the blood vessel that keeps it alive.
Surgeons carrying out flap reconstruction use either local flaps, which remain connected to their blood supply, or free flaps, which are separated from their source and require reconnection of the blood vessels under a microscope at the recipient site.
All procedures are carried out under general anaesthetic and can last several hours depending on the severity of the injury.
Reconstruction using local flaps can often take place at the same time as bone fixation. In the image above, a muscle from the calf is transferred, keeping its blood supply in tact to cover an open fracture below the knee.This is called a gastrocnemius muscle flap, taking its name from the muscle that has been moved.
Is this surgery available on the NHS?
Orthopaedic surgery and reconstructive plastic surgery to repair open fractures of the lower limb are widely available on the NHS.
Who will I see as patient?
As an open fracture patient, you will be seen by a multi-disciplinary team. This team will be made up of specialists working together to make sure that the best possible treatment is given. These specialists may include the following:
• Orthopaedic surgeon
• Plastic surgeon
• Physiotherapist
What should I expect in terms of treatment, procedures and outcomes?
Patients undergoing surgery for an open fracture can expect a good functional return in terms of bone healing and repair, with a 90% success rate in most cases.
However, treatment can be prolonged, especially for patients treated with circular frames and undergoing bone lengthening.Patients should remember, however, that even in the best hands there will be scarring following open fracture surgery. The procedures described in this section are all about restoring function, not form, and due to the loss of tissue and the use of flaps and skin grafts, some scarring is inevitable.
Some patients may find that they have reduced exercise tolerance following open fracture surgery, and may not be able to play certain sports as well as they once did, but a return to everyday function is highly likely. With good healing and rehabilitation procedures, 80% of patients get back to some form of employment, although the bone healing period of many months (often 6-9 months or more depending on the type of injury) can have a major impact on people’s lives. On average, patients may expect to get back approximately 75% of their leg function. Patients can also experience pain and discomfort during this period of recovery.
For this reason, and in cases where limb damage is severe, an amputation can be the best treatment option. With the advancements in prosthetic limb technology, can promise a far quicker return to normal life. Scenarios where an amputation may be considered is when there are extensive injuries to the foot, loss of a large segment of the tibia (the major bone in the leg) and extensive muscle or nerve loss or if the leg has had no blood supply for a prolonged period.